Introduction
Virtual-Reality Treatment for First Responder PTSD: A Pilot Investigation Across the globe, traumatic events are witnessed by a significant percentage of the general population (Benjet et al., 2016), yet some occupations place individuals at higher risk for exposure, and repeated exposure, to trauma and thus, to the development of PTSD. One such group at high risk are first responders, who a) are exposed to traumatic events at significantly higher rates than the general population and b) are at higher risk for the development of PTSD, with rates ranging from 6% to 32% for law enforcement officers, 9%–22% for emergency medical technicians/paramedics, and 17%–32% for firefighters (Lewis-Schroeder et al., 2018). These rates are substantially higher than the rates of PTSD in the general adult population (7%–12%; Lewis-Schroeder et al., 2018). Furthermore, first responders are more likely to die by suicide than in the line of duty (Ruderman Foundation, 2018), and they die by suicide at higher rates than the general population. First responders also had higher lifetime rates of suicidal ideation (63.2%) than non-first responders (36.8%; Bond and Anestis, 2023). Given the link between PTSD and suicide (e.g., May and Klonsky, 2016) and that PTSD treatment reduces risk for suicide (Rozek et al., 2022), understanding how to help first responders, a group at high risk of negative mental health outcomes, through evidence-based treatment and prevention services is needed.
Despite their high risk and increasing recognition of the toll that the first responder occupation can take on their emotional health, there are only limited data on the efficacy of psychological treatment for this population. A systematic review of the treatment literature (Alden et al., 2020) found 10 treatment outcome investigations, eight of which were randomized controlled trials (RCT). However, only one RCT was considered to be of high quality (Bryant et al., 2018). In that investigation, first responders diagnosed with PTSD received a cognitive-behavioral treatment (CBT) that included psychoeducation and four sessions of skills training (management of comorbid symptoms/behaviors of depression, panic, emotion regulation, substance use, anger or interpersonal relationships depending on patient need). In addition, participants were randomized to 12 weekly sessions of cognitive-behavior therapy–long (CBT-L; including 40 min of prolonged exposure), 12 weekly sessions of cognitive-behavior therapy–brief (CBT-B; including 10 min of exposure therapy), or a wait-list control condition. The results indicated that both CBT groups resulted in a greater reduction in PTSD scores on the Clinician Administered PTSD Scale (DSM-IV version). At posttreatment, 40.7% of the CBT-L group still met diagnostic criteria for PTSD, compared to 24.1% of the CBT-B group and 89.3% of the wait-list group. Treatment outcomes for the two CBT conditions were maintained 6-month follow-up.
Since the Alden and colleagues (2020) review, there have been at least two additional treatment studies conducted with samples of firefighters with PTSD. Meyer et al. (2022) reported the treatment outcome of 15 firefighters who screened positive for PTSD using the PTSD Checklist for DSM-5 (PCL-5; Weathers et al., 2013) and were treated with the Unified Protocol for Transdiagnostic Treatment of Emotional Disorders via videoconferencing. There was a significant decrease in PCL-5 scores at posttreatment, and the results were maintained at 1 month follow-up. Although the mean PCL-5 score at post treatment decreased by 15.9 points and met the criteria for clinically reliable change (Marx et al., 2022), the number of participants no longer meeting DSM-5 criteria for PTSD was not provided. Additionally, Zwetig et al. (2022) reported positive treatment outcome for two firefighters meeting diagnostic criteria for PTSD using massed prolonged exposure. Both participants made positive improvement, although one participant had an increase in self-reported PTSD symptoms at 1 month follow-up relative to the end of treatment.
An additional challenge for exposure therapy is the significant drop-out rate that occurs because of once weekly or sometimes, once monthly treatment (Kehle-Forbes et al., 2016; Eftekhair et al. 2020). Similar to military populations, Bryant et al. (2018) reported that 33% of the participants in their CBT-L group and 27% of participants in their CBT-B group participated in fewer than eight of the planned 12 to 14 treatment sessions (i.e., received only 50% of the allocated intervention). Effective treatments are not effective if first responders cannot avail themselves of the intervention.
These issues converge to indicate a need to identify an efficient, effective intervention for PTSD among first responders. One approach that seems promising in this regard is Intensive Outpatient Programs (IOPs). Instead of weekly sessions, these programs typically offer treatment in a condensed format that aims to complete treatment more quickly, often in two or 3 weeks (Ragsdale, Watkins, Sherill, Zwiebach and Rothbaum, 2020). In addition to the shortened treatment length, these programs have also been associated with increased retention (Ragsdale et al., 2020).
One therapeutic approach that seems well suited to IOP is exposure therapy. For example, in a series of investigations, our research center demonstrated that a 3-week intensive outpatient program (IOP), using daily exposure therapy treatment, augmented by virtual reality, is efficacious in treating military PTSD (Beidel et al., 2017; Beidel et al., 2019), with 66% of individuals no longer meeting diagnostic criteria for PTSD at posttreatment and a drop-out rate of 2%. Other studies have reported similarly positive results using exposure therapy in an IOP format (see Ragsdale, et al., 2020 for a review). However, these studies have been conducted largely with military personnel. No studies of exposure-based IOPs have been reported to the best of our knowledge.
While first responders share many characteristics with active-duty military personnel, there are important differences that require empirical validation of IOP-based exposure therapy for this group. For example, first responders are often exposed to multiple traumas–often vicariously. This exposure is different than the (relatively) isolated self-focused exposures often reported by military members. Furthermore, first responders are likely to encounter a much greater variety of potentially traumatizing events during the course of their career. Furthermore, it has been reported that job-related physical injuries are more likely to be related to PTSD in first responders than in military personnel (Obuobi-Donkor, Oluwasina, Nkire and Agyapong, 2022).
As a result of a) the positive outcome with military personnel, b) the increasing recognition that first responders experience mental health problems at a rate similar to military veterans, and c) the mass casualty events that occurred in Florida over the past 7 years (mass shootings, Category four hurricanes), a treatment program was developed to provide services to first responders. However, at that time, there was no virtual reality program available that consisted of scenes depicting traumatic events encountered by first responders. Thus, the first step was to develop a VR system for this population and then to examine the feasibility, acceptability and initial efficacy of exposure therapy for the treatment of first responder PTSD.
In this investigation, we present a pilot investigation of exposure therapy, augmented by the use of the new virtual reality system, for the treatment of PTSD in first responders. Based on the small extant literature, we hypothesized that this intervention, presented in an intensive outpatient fashion, would be feasible, acceptable and efficacious for this population. The second hypothesis was that these improvements would be maintained at 3-month follow-up.
Methods
Participants
The study was approved by the Unied States Army Medical Research and Materiel Command (USAMRMC), Office of Research Protections (ORP), Human Research Protection Office and the University of Central Florida Institutional Review Board, where treatment took place. Informed consent was obtained from each participant. Participants were recruited through clinician or self-referral, social media ads, and presentations at local health and mental health fairs. Potential participants had to be 18 years or older and had experienced a traumatic event related to their work as a first responder. Other exclusion criteria included a) acute cardiac difficulties (angina, myocardial infarction, and severe hypertension) unless medically cleared by a physician to participate in exposure therapy, b) history of seizures (due to the potential for VR to initiate seizure activity); c) diagnosis of antisocial personality disorder or a current diagnosis of psychosis or substance use disorder rated as severe; d) PTSD symptoms lasting less than 6 months; e) use of benzodiazepines unless willing to discontinue under physician guidance. Use of other psychotropic medications was not exclusionary, but the dosage had to remain stable throughout the course of treatment. A total of 19 participants completed treatment, with 15 completing at least one measure through follow-up and being included in the analysis. Eight of the sample were law enforcement officers, and seven were firefighters/paramedics. Demographic data are presented in Table 1.
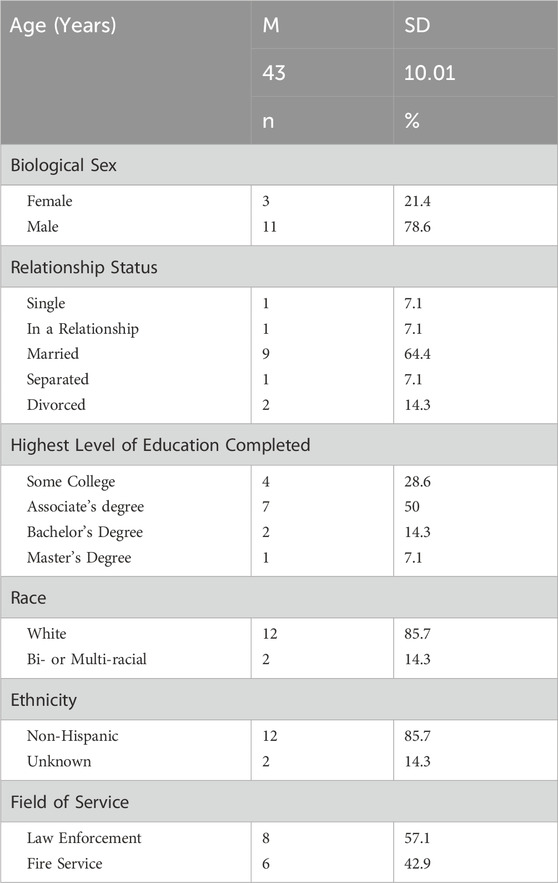
Table 1. Demographic data.
Assessment measures
Feasibility and acceptability of intensive VR treatment
Simulator Sickness Questionnaire (Kennedy et al., 1993). This questionnaire assesses various physical reactions that may occur as a result of simulation or virtual reality environments. Each symptom is rated on a four-point severity scale from 0 (none) to 3 (severe). This measure was administered at the end of each treatment session.
Clinician Checklist. This checklist was administered at the start of each treatment session to track iatrogenic effects often believed to result from intensive treatment for trauma. Behaviors tracked included the presence of any suicidal ideation/attempts, number of alcoholic drinks since the last treatment session (as a marker of substance use), and number of anger outbursts.
Treatment outcome
The following measures were administered at pre-treatment, post-treatment, and 3-month follow-up.
Clinician-Administered PTSD Scale for DSM-5 (CAPS; Weathers et al., 2013). The CAPS-5 is a structured clinician administered diagnostic interview that assesses symptoms of PTSD within the past month. The CAPS-5 has high interrater reliability for PTSD diagnosis (κ = .78 to 1.00) and total severity score (ICC = .91), good test-retest reliability for PTSD diagnosis (κ = .83) and severity score (ICC = .78), good internal consistency for severity items (α = .88) and good convergent and discriminant validity (Weathers et al., 2013). This measure was administered at pre-treatment, post-treatment, and 3-month follow-up.
Posttraumatic Stress Disorder Checklist for DSM-5 (PCL-5; Weathers et al., 2013). The PCL-5 is a self-report measure of DSM-5 PTSD symptoms, which are rated on a severity scale from 0 (not at all) to four (extremely). Initial studies demonstrated that PCL-5 scores are reliable and valid measures of PTSD symptoms (Blevins, Weathers, Davis, Witte and Domino, 2015). In a recent study with veterans, PCL-5 scores were shown to have excellent internal consistency (α = .96) and good test-retest reliability (r = .84); convergent and discriminant validity were also demonstrated (Bovin et al., 2016). This measure was administered at all assessment points.
World Health Organization Disability Assessment Schedule 2.0 (WHODAS 2.0; Üstün et al., 2010). The WHODAS 2.0 is a 36-item measure of impairment that assesses six domains of physical or mental health (cognition, mobility, self-care, getting along with people, life activities, and participation in society). Participants rate each item from “none” to “extreme or cannot do.” Good internal consistency has been demonstrated for all subscales, test-retest reliability is also moderate to good at the item level and excellent at the domain level, and concurrent validity was demonstrated (Üstün et al., 2010). This measure was administered at all assessment time points.
Quality of Life Scale (QOLS; Burckhardt and Anderson, 2003). The QOLS is a 16-item measure assessing the subjective quality of six domains of life: independence, recreation, personal development and fulfillment, material and physical wellbeing, relationships with others, and community and civic involvement. Patients rate the items on the QOLS on a seven-point Likert scale from 1 (terrible) to 7 (delighted). This measure was administered at all assessment time points.
Patient Health Questionnaire-9 (PHQ-9; Kroenke and Spitzer, 2002). The PHQ-9 is a nine-item self-report measure of depression symptoms. Participants rate each item on a 0 (not at all) to 3 (nearly every day) scale. Scores from the PHQ-9 have been shown to be reliable and valid (Kroenke and Spitzer, 2002; Titov et al., 2011). This measure was administered at all assessment time points.
Generalized Anxiety Disorder-7 (GAD-7; Spitzer et al., 2006). The GAD-7 is a seven-item self-report measure of general anxiety symptoms. Participants rate each item on a 0 (not at all) to 3 (nearly every day) scale. Reliability and validity of scores from the GAD-7 has been established (Spitzer et al., 2006; Löwe et al., 2008). This measure was administered at all assessment points.
Dimensions of Anger Reactions-5 (DAR-5; Forbes, Alkemade, Mitchell, et al., 2014a). The DAR-5 is a five-item measure, where each item is rated on a 1 (none or almost none of the time) to 5 (all or almost all of the time) scale. The reliability and validity of scores from the DAR-5 has been established in university, trauma-exposed, and veteran samples (Forbes, Alkemade, Mitchell, et al., 2014a; Forbes, Alkemade, Hopcraft, et al., 2014b). This measure was administered at all assessment points.
Treatment
Traumatic events included responding to mass casualty situations such as the Pulse nightclub shooting and the Champlain Towers condominium collapse in Surfside, FL as well as more common traumatic events such as pediatric deaths and murder-suicide investigations. All patients were treated in an intensive 10-day treatment protocol (5 days per week for 2 weeks with no treatment occurring on weekends) that consisted of individual exposure therapy augmented with virtual reality. After completing the pre-treatment assessment, the clinician conducted a detailed interview with the patient, to get the specifics regarding their traumatic event, including thoughts, emotions, behaviors that occurred during the time of the event as well as sights and sounds that served as triggers for PTSD symptoms including anxiety and avoidance behaviors. Using all of that information, an individualized VR scenario was constructed for use in the exposure treatment.
Treatment was conducted by master’s level clinicians who had previously received extensive training experience conducting exposure therapy with virtual reality for military populations within this same clinic setting. Participants were randomized to one of two treatment conditions–session length of 45 min or session length continues until within session habituation occurs, although it remains unclear whether within session habituation is necessary factor for overall successful treatment outcome (Sripada and Rauch, 2015 for an excellent discussion of this issue). This design allowed us to examine whether the system was equally effective for fixed session lengths (typical in Prolonged Exposure) and unbounded session lengths (used in Trauma Management Therapy).
Regardless of treatment condition assignment, each session was conducted in an identical fashion with the exception of treatment length. The patient was provided with a head mounted display and the clinician initiated the exposure session by beginning the virtual reality scenario. At the same time, the therapist read aloud the traumatic event, consistent with traditional forms of imaginal exposure therapy. In other words, in traditional imaginal exposure, the therapist reads the scene while the patient imagines the scene. In exposure therapy augmented with VR, the therapist reads the scene while the patient watches and listens to the VR.
At 10 min intervals, the therapist queried the patient as to their emotional distress, using a nine point Subjective Units of Distress Scale, where eight indicated extreme distress, 4 = moderate distress, and 0 = no distress. In the unbound condition, treatment continued until the patient reported a distress rating that was 50% lower than the session peak. In the 45 min condition, the session was ended after 45 min, regardless of SUDS level.
The treatment sessions averaged 62.27 (SD = 25.92) minutes across conditions. Additionally, patients were given daily homework assignments consisting of in vivo exposure to situations or behaviors that they avoided as a result of their traumatic event. Such assignments included returning to the place of the traumatic event or if relevant, a similar situation or activities avoided due to hypervigilance and remaining there until any anxiety they experienced had dissipated.
Virtual reality system
Developed using Unity (v. 2019.3.14f1), the TraumaVR Creation System allows clinicians to recreate trauma scenarios using an intuitive, screen-based interface. The system consists of a PC capable of running VR and an internet connection, two monitors that support a screen resolution of 1920 × 1,080, and standard peripherals such as a mouse, keyboard, and speakers. A headset, such as the Oculus Rift (preferred) or HTC Vive is also required. The system runs using Steam VR. Furthermore, the system has the capability to collect physiological data, such as heart rate and skin conductance.
Upon initiating the program, the clinician can choose from over 40 pre-existing environments where previous patients have experienced traumatic events including a) interior spaces (bedrooms, motel rooms, bathrooms), b) exterior locations (roadsides, parking lots, swimming pools), c) military based and combat situations, and d) nationally known traumatic event locations such as the Pulse Nightclub in Orlando, Florida and Champlain Towers in Surfside, Florida. If an environment does not exist, the system allows its creation. Once the environment is selected/created, the clinician can further customize it using a simple interface, including visual elements such as time of day, color of interior furnishings and decorative elements, and patient perspective. Ambient sounds may also be added, such as a fan, crickets, a barking dog, wind, and rain. There is also the capability to include smells that may serve as triggers for emotional distress and add up to five characters, who are relevant to the traumatic event, including assigning sex, weight, eye color, hair color and style, clothing, and shoes. Characters can be animated or static, depending on the traumatic event details.
The system uses dual monitors. The left monitor contains the interface that allows the clinician to play, pause, and create loops in the playback of the trauma scenario. The monitor also displays the trauma narrative (i.e., the written description of the traumatic event), an area for notes or additional details, quick access to the release of smells and sounds, and the ability to log SUDS ratings, using the 0 through eight keys on their keyboard. The right-hand monitor displays what the patient sees in the headset. There is also an option to display the patient’s real time heart rate and electrodermal activity if that option and the necessary physiological equipment is selected. All data collected during the exposure session are uploaded into an. xml file on the clinician’s machine and can be stored in a separate database. An example of the clinician interface is provided in Figure 1. An example of the patient’s view is provided in Figure 2.
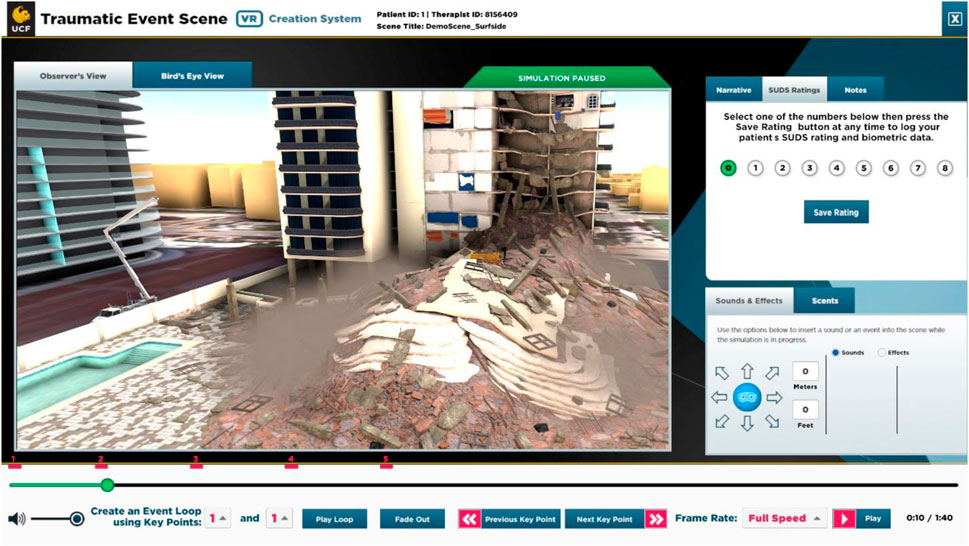
Figure 1. Sample clinician screen.
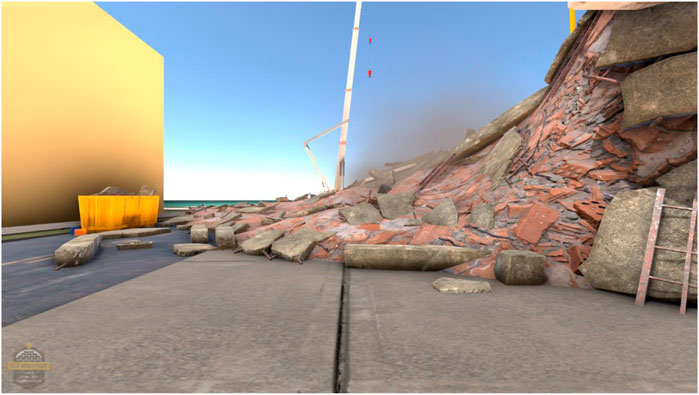
Figure 2. Sample patient view.
Results
Feasibility and acceptability of intensive outpatient treatment
No patient dropped out of the study for any reason, including believing that the daily treatment was too onerous. None of the first responders had to be removed from the study due to self-reported worsening PTSD symptoms. Additionally, the number of patients experiencing symptoms of simulator sickness was low (see Table 2). Out of the 190 exposure sessions provided, no individual experienced symptoms severe enough for the session to be ended early, such as severe motion sickness or severe headache.
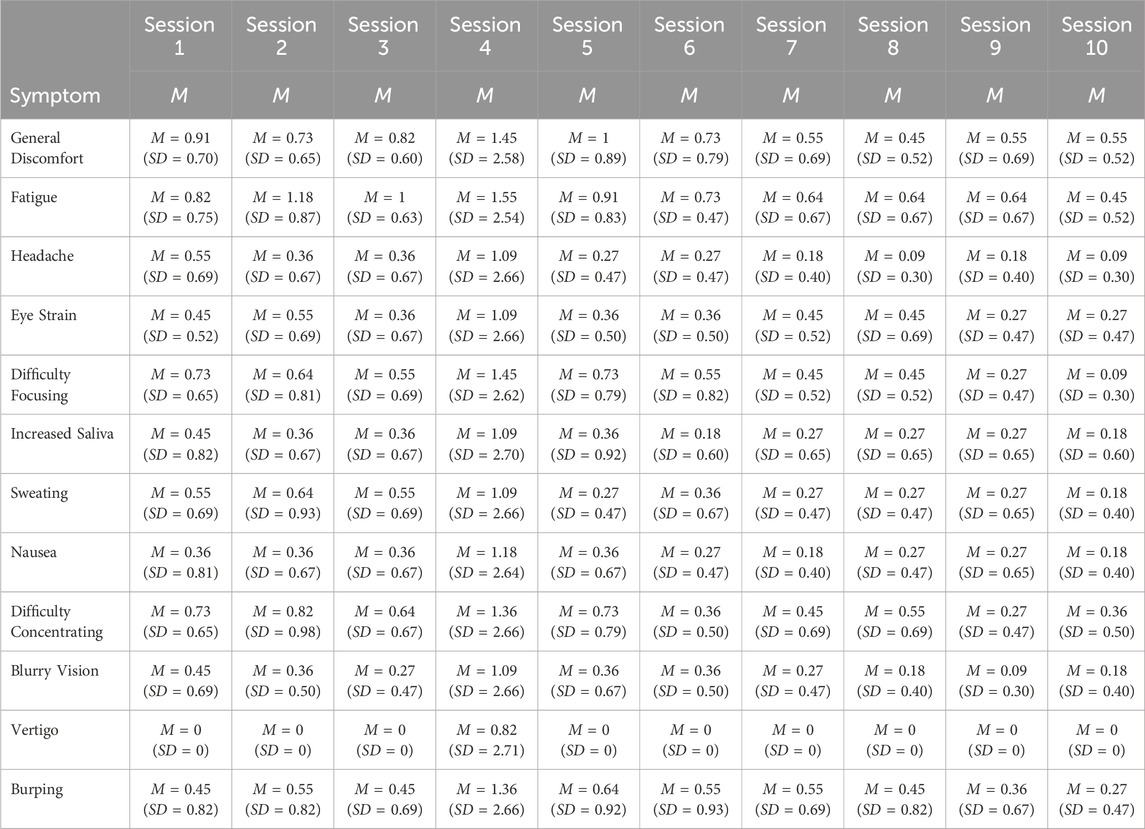
Table 2. Mean levels of simulator sickness at each session (N = 11).
Iatrogenic effects of intensive outpatient treatment
IOP treatment required daily sessions of exposure therapy, augmented by VR, and daily homework assignments (as described above). It is possible that such intensive treatment could lead to general emotional distress from having to confront the trauma on a daily basis. To track any iatrogenic effects, patients were asked to report whether they experienced any anger outbursts, whether they experienced suicidal ideation, and how many alcoholic drinks they consumed since the previous session daily. As illustrated in Table 3, all of these behaviors occurred at a very low frequency within this group of participants and did not show any trend to indicate increasing distress as a result of daily exposure treatment for PTSD.
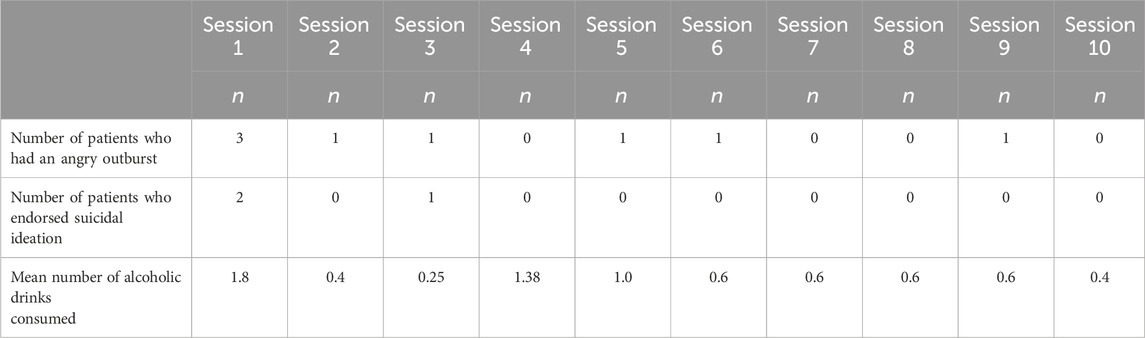
Table 3. Frequency of iatrogenic effects during intensive treatment (N = 13).
Treatment outcome
Outcome variables were analyzed using generalized linear modeling, examining the effect time at pre, post, and 3-month follow-up. Mean scores for both groups at all time periods are presented in Table 4.
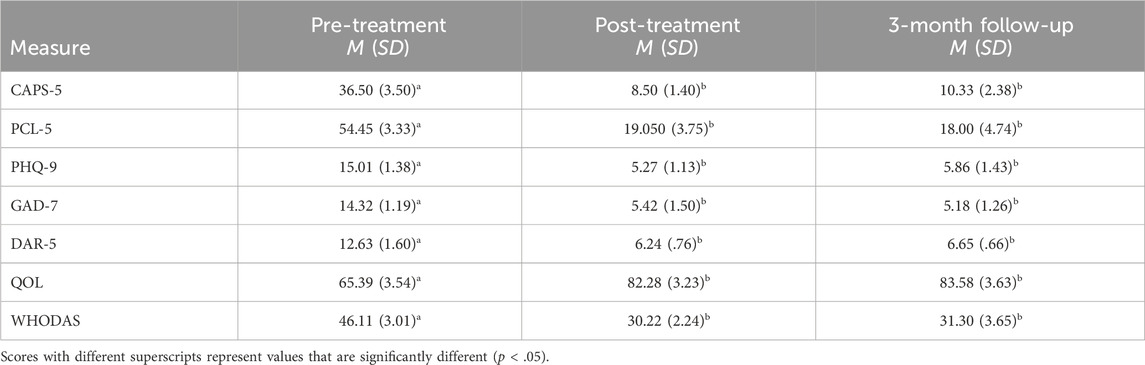
Table 4. Scores on treatment outcome measures at pre- and post-treatment and 3-month follow-up.
PTSD measures
CAPS-5. Fourteen participants completed the CAPS-5 through follow-up and were used in the analysis. The results of the 2 (Condition) x 3 (Time) mixed ANOVA revealed that there was no main effect of condition [F (1,12) = .158, p = .69] There was a significant main effect for time [F (1,12) = 76.63, p < .001, ηp2 = .92]. There was a significant decrease in CAPS-5 scores from pre-to post-treatment, and that improvement was maintained at 3-month follow-up. However, there was not a significant interaction between condition and time [F (2, 12) = .529, p = .60].
Based on the posttreatment CAPS-5 interview, none of the participants met diagnostic criteria for PTSD at the end of the treatment. Furthermore, treatment gains were maintained, and no participant met diagnostic criteria for PTSD at 3-month follow-up.
PCL-5.15 participants completed the PCL-5 through follow-up. A similar 2 × 3 mixed ANOVA revealed no significant main effect of condition [F (1,13) = 1.21, p = .66]. There was a significant main effect for time [F (1, 13) = 80.61, p < .001, ηp2 = .86]. There was a significant decrease in PCL-5 scores from pre-to post-treatment, and that improvement was maintained at 3-month follow-up. There was not a significant condition × time interaction [F (1, 13) = .77, p = .40].
Assessment of related emotional distress
PHQ-9. Twelve participants completed the PHQ-9 through follow-up. The results of the ANOVA revealed no main effect of condition [F (1,10) = .30, p = .60]. There was a significant main effect for time [F (2, 10) = 44.30, p < .001, ηp2 = .82] with a significant decrease in depressive symptoms from pre-to post-treatment, and improvement was maintained at 3-month follow-up. There was not a significant interaction between Condition and time (F (2,10) = 1.33, p = 37).
GAD-7. Fourteen participants completed the GAD-& through follow-up. The ANOVA revealed no main effect for condition [F (1,12) = .66, p = .43]. Once again, there was a significant main effect for time [F (2, 12) = 25.14, p < .001, ηp2 = .69]. GAD-7 scores decreased significantly from pre-to post-treatment, and that improvement was maintained at 3-month follow-up. There was no significant interaction between condition and time (F (2, 12) = .635, p = .54).
DAR-5. Thirteen participants completed the DAR-5 through follow-up. The 2 × 3 mixed ANOVA indicated no main effect of condition [F (1, 11) = .23, p = .64]. There was a significant main effect for time on the DAR-5 [F (2, 11) = 18.48, p < .001, ηp2 = .63]. There was not a significant interaction between condition and time [F (, 11) = .493, p = .62]. Again, there was a significant decrease in anger scores from pre-to post-treatment, and that improvement was maintained at 3-month follow-up.
Quality of life and functional impairment
QOL. 15 participants completed the QOL through follow-up. The ANOVA results for the QOL revealed no significant main effect of condition [F (1,13) = .26, p = .66]. There was a significant main effect for time [F (2,13) = 19.77, p < .001, ηp2 = .60], with a significant increase in QOL scores from pre-to post-treatment and maintained at 3-month follow-up. Finally, there was not a significant interaction between condition and time [F (2, 13) = .55, p = .47].
WHODAS. Fourteen participants completed the WHODAS through follow-up. The ANOVA revealed no significant main effect for condition [F (1, 12) = .16, p = .70). There was a significant main effect for time [F (2,11) = 17.58, p < .001, ηp2 = .59]. There was a significant decrease in WHODAS scores from pre-to post-treatment, and that improvement was maintained at 3-month follow-up. The interaction between condition and time was not significant [F (2, 11) = .01, p = .91].
Discussion
In 2020, there were an estimated 1,041,200 career and volunteer firefighters in the United States (Fahy et al., 2022). Similarly, there were over one million public safety officers in the United States—906,037 full-time law enforcement employees and 94,275 part-time employees (usafacts.org). Despite the increasing recognition that first responders experience multiple traumatic events and are at increased risk for suicide (see Johnson et al., 2019, for a review), there are few data addressing the treatment of trauma and PTSD in this population.
Building on the need to address the stigma of treatment and prior success with military populations, this study represents the first trial of a 2-week IOP with first responders, using exposure therapy augmented by VR. The results demonstrated that such an intensive program is feasible to implement and acceptable to the participants. The 0% drop-out rate for this study may reflect the small sample size but is consistent with our previous investigation with a much larger sample size (2%; Beidel et al., 2017) and lower than other investigations with military populations (33%–44%; see Beidel et al., 2017) and first responders (18%–33%; Bryant et al., 2018; Meyer et al., 2022). Furthermore, the patients reported minimal simulation sickness as a result of using the VR system (45–60 min of exposure therapy duration) and no iatrogenic effects as a result of 10 days of intensive treatment.
Using a 2-week treatment protocol, ten sessions of exposure therapy, augmented with virtual reality, and in vivo exposure homework assignments was associated with positive treatment outcomes in a pilot study of first responders seeking treatment for PTSD. Consistent with other investigations (Bryant et al., 2018; Meyer et al., 2022; Zwetig et al., 2022), scores significantly decreased at posttreatment on self-report and clinician-assessed PTSD as well as associated measures of psychopathology, such as anger, anxiety, and depression. Additionally, patients in the current investigation reported significantly reduced disability as well as enhanced quality of life, and all treatment gains were maintained at 3-month follow-up. Furthermore, in this investigation, none of the patients met diagnostic criteria for PTSD at posttreatment or follow-up, in comparison to the 24.1%–40.7% for CBT-B and CBT-L (Bryant et al., 2018). Although the reasons for this difference are unclear, it may be that the focus on one intervention (exposure therapy) delivered at full strength may be most effective at eliminating the core symptoms of PTSD, rather than delivering a combination of CBT skills that may not capture the entirety of the treatment. An alternative hypothesis is that the use of virtual reality augments traditional exposure therapy as there is no need to rely on the patient’s imagination in order to present them with the important traumatic cues. Patients may be able to imagine, albeit reluctantly, visual memories of the event. However, imagining sounds and smells are more difficult. The use of virtual reality allows those cues to be presented directly, and at higher intensity, possibly allowing for a better treatment outcome. Of course, direct comparisons of these different approaches (CBT package vs VR augmented exposure therapy vs exposure therapy without VR) would be necessary in order to actually answer this question.
As with any other investigation, this study has its limitations. First, as a pilot investigation, there was no control group; however, epidemiological data provide support that PTSD, particularly when following war related trauma or physical violence, does not spontaneously remit (Kessler et al., 2017). The mass casualties and everyday physical traumas witnessed by first responders would fall into these categories. A second limitation is the small sample size. Although much smaller than one investigation (Bryant et al., 2018), this sample size was equivalent to or larger than two other investigations with first responders (Meyer et al., 2022; Zwetig et al., 2022). Clearly, larger samples and more investigations are needed. However, given the stigma that prevents first responders from asking for help, every study that can demonstrate positive treatment outcome will counter not only the stigma about seeking treatment (First Responder Task Force Report, 2021) but also the belief that treatment will result in negative outcomes (Johnson et al., 2019).
In conclusion, the results of this pilot study demonstrate that a 2-week IOP that uses exposure therapy augmented by virtual reality is a feasible, acceptable, and efficacious treatment for PTSD in a sample of first responders. The use of this short but intensive treatment program resulted in treatment gains that were maintained 3 months later, with 100% of the sample losing their diagnosis of PTSD at post-treatment and no relapse at follow-up. The use of treatments with a strong evidence base but presented in an innovative fashion may serve to help break the stigma of seeking treatment, allowing first responders seek and receive the treatments that they deserve.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by Institutional Review Board—University of Central Florida. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
DB: Writing–original draft, Writing–review and editing. CB: Writing–original draft, Writing–review and editing. AN: Writing–review and editing, Writing–original draft. CS: Writing–original draft, Writing–review and editing. DR: Writing–original draft, Writing–review and editing. CM: Writing–original draft. DH: Writing–review and editing.
Funding
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. This research was supported by a Department of Defense contract W81XWH18C0164 to the first, second, and third authors.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
Alden, L. E., Matthew, L. R., Wagner, S., Fyfe, T., Randall, C., Regehr, C., et al. (2020). Systematic literature review of psychological interventions for first responders. Work Stress 35 (2), 193–215. doi:10.1080/02678373.2020.1758833
CrossRef Full Text | Google Scholar
Beidel, D. C., Frueh, B. C., Neer, S. M., Bowers, C. A., Trachik, B., Uhde, T. W., et al. (2019). Trauma Management Therapy with virtual-reality augmented exposure therapy for combat-related PTSD: a randomized controlled trial. J. Anxiety Disord. 61, 64–74. doi:10.1016/j.janxdis.2017.08.005
PubMed Abstract | CrossRef Full Text | Google Scholar
Beidel, D. C., Frueh, B. C., Neer, S. M., and Lejuez, C. W. (2017). The efficacy of Trauma Management Therapy: a controlled pilot investigation of a three-week intensive outpatient program for combat-related PTSD. J. Anxiety Disord. 50, 23–32. doi:10.1016/j.janxdis.2017.05.001
PubMed Abstract | CrossRef Full Text | Google Scholar
Benjet, C., Bromet, E., Karam, E. G., Kessler, R. C., McLaughlin, K. A., Ruscio, A. M., et al. (2016). The epidemiology of traumatic event exposure worldwide: results from the World Mental Health Survey Consortium. Psychol. Med. 46, 327–343. doi:10.1017/S0033291715001981
PubMed Abstract | CrossRef Full Text | Google Scholar
Blevins, C. A., Weathers, F. W., Davis, M. T., Witte, T. K., and Domino, J. L. (2015). The posttraumatic stress disorder checklist for DSM-5 (PCL-5): development and initial psychometric evaluation. J. Trauma. Stress 28 (6), 489–498. doi:10.1002/jts.22059
PubMed Abstract | CrossRef Full Text | Google Scholar
Bond, A. E., and Anestis, M. D. (2023). Understanding capability and suicidal ideation among first responders. Archives Suicide Res. 27 (2), 295–306. doi:10.1080/13811118.2021.1993397
CrossRef Full Text | Google Scholar
Bovin, M. J., Marx, B. P., Weathers, F. W., Gallagher, M. W., Rodriguez, P., Schnurr, P. P., et al. (2016). Psychometric properties of the PTSD checklist for diagnostic and statistical manual of mental disorders–fifth edition (PCL-5) in veterans. Psychol. Assess. 28 (11), 1379–1391. doi:10.1037/pas0000254
PubMed Abstract | CrossRef Full Text | Google Scholar
Bryant, R. A., Kenny, L., Rawson, N., Cahill, C., Joscelyne, A., Nickerson, A., et al. (2018). Efficacy of exposure-based cognitive behaviour therapy for post-traumatic stress disorder in emergency service personnel: a randomised clinical trial. Psychol. Med. 49, 1565–1573. doi:10.1017/S0033291718002234
PubMed Abstract | CrossRef Full Text | Google Scholar
Eftekhair, A., Crowley, J. J., Mackintosh, M. A., and Rosen, C. S. (2020). Predicting treatment dropout among veterans receiving prolonged exposure therapy. Psychol. Trauma Theory, Res. Pract. Policy 12 (4), 405–412. doi:10.1037/tra0000484
CrossRef Full Text | Google Scholar
Forbes, D., Alkemade, N., Hopcraft, D., Hawthorne, G., O’Halloran, P., Elhai, J. D., et al. (2014a). Evaluation of the Dimensions of Anger Reactions-5 (DAR-5) Scale in combat veterans with posttraumatic stress disorder. J. Anxiety Disord. 28 (8), 830–835. doi:10.1016/j.janxdis.2014.09.015
PubMed Abstract | CrossRef Full Text | Google Scholar
Forbes, D., Alkemade, N., Mitchell, D., Elhai, J. D., McHugh, T., Bates, G., et al. (2014b). Utility of the Dimensions of Anger Reactions–5 (DAR-5) scale as a brief anger measure. Depress. Anxiety 31 (2), 166–173. doi:10.1002/da.22148
PubMed Abstract | CrossRef Full Text | Google Scholar
Kehle-Forbes, S. M., Meis, L. A., Spoont, M. R., and Polusny, M. A. (2016). Treatment initiation and dropout from prolonged exposure and cognitive processing therapy in a VA outpatient clinic. Psychol. Trauma Theory, Res. Pract. Policy 8 (1), 107–114. doi:10.1037/tra0000065
PubMed Abstract | CrossRef Full Text | Google Scholar
Kessler, R. C., Aguliar-Gaxiola, S., Alonson, J., Benjet, C., Bromet, E., Cardoso, G., et al. (2017). Trauma and PTSD in the who world mental health surveys. Eur. J. Psychotraumatology 27 (8Suppl. 5), 1353383. doi:10.1080/20008198.2017.1353383
PubMed Abstract | CrossRef Full Text | Google Scholar
Kroenke, K., and Spitzer, R. L. (2002). The PHQ-9: a new depression diagnostic and severity measure. Psychiatr. Ann. 32 (9), 509–515. doi:10.3928/0048-5713-20020901-06
CrossRef Full Text | Google Scholar
Kubany, E. S., Haynes, S. N., Abueg, F. R., Manke, F. P., Brennan, J. M., and Stahura, C. (1996). Development and validation of the trauma-related guilt inventory (TRGI). Psychol. Assess. 8 (4), 428–444. doi:10.1037//1040-3590.8.4.428
CrossRef Full Text | Google Scholar
Lewis-Schroeder, N. F., Kieran, K., Murphy, B. L., Wolff, J. D., Robinson, M. A., and Kaufman, M. L. (2018). Conceptualization, assessment and treatment of traumatic stress in first responders: a review of critical issues. Harv. Rev. Psychiatry 26 (4), 216–227. doi:10.1097/HRP.0000000000000176
PubMed Abstract | CrossRef Full Text | Google Scholar
Löwe, B., Decker, O., Müller, S., Brähler, E., Schellberg, D., Herzog, W., et al. (2008). Validation and standardization of the generalized anxiety disorder screener (GAD-7) in the general population. Med. Care 46, 266–274. doi:10.1097/mlr.0b013e318160d093
PubMed Abstract | CrossRef Full Text | Google Scholar
May, A. M., and Klonsky, E. D. (2016). What distinguishes suicide attempters from suicide ideators? A meta-analysis of potential factors. Clin. Psychol. Sci. Pract. 23 (1), 5–20. doi:10.1111/cpsp.12136
CrossRef Full Text | Google Scholar
Meyer, E. C., Coe, E., Pennington, M. L., Cammarata, C., Kimbrel, N. A., Ostiguy, W., et al. (2022). The Unified Protocol for Transdiagnostic Treatment of Emotional Disorders delivered to firefighters via videoconferencing: pilot outcomes highlighting improvements in alcohol use disorder and posttraumatic stress disorder symptoms. Cognitive Behav. Pract. 31, 215–229. doi:10.1016/j.cbpra.2022.08.004
CrossRef Full Text | Google Scholar
Obuobi-Donkor, G., Oluwasina, F., Nkire, N., and Agyapong, V. I. (2022). A scoping review on the prevalence and determinants of post-traumatic stress disorder among military personnel and firefighters: implications for public policy and practice. Int. J. Environ. Res. public health 19 (3), 1565. doi:10.3390/ijerph19031565
PubMed Abstract | CrossRef Full Text | Google Scholar
Ragsdale, K. A., Watkins, L. E., Sherrill, A. M., Zwiebach, L., and Rothbaum, B. O. (2020). Advances in PTSD treatment delivery: evidence base and future directions for intensive outpatient programs. Curr. Treat. Options Psych. 7, 291–300. doi:10.1007/s40501-020-00219-7
CrossRef Full Text | Google Scholar
Rozek, D. C., Baker, S. N., Rugo, K. F., Steigerwald, V. L., Sippel, L. M., Holliday, R., et al. (2022). Addressing co-occurring suicidal thoughts and behaviors and posttraumatic stress disorder in evidence-based psychotherapies for adults: a systematic review. J. Trauma. Stress 35 (2), 729–745. doi:10.1002/jts.22774
PubMed Abstract | CrossRef Full Text | Google Scholar
Spitzer, R. L., Kroenke, K., Williams, J. B., and Löwe, B. (2006). A brief measure for assessing generalized anxiety disorder: the GAD-7. Archives Intern. Med. 166 (10), 1092–1097. doi:10.1001/archinte.166.10.1092
PubMed Abstract | CrossRef Full Text | Google Scholar
Sripada, R. K., and Rauch, S. A. M. (2015). Between-session and within-session habituation in Prolonged Exposure Therapy for posttraumatic stress disorder: a hierarchical linear modeling approach. J. Anxiety Disord. 30, 81–87. doi:10.1016/j.janxdis.2015.01.002
PubMed Abstract | CrossRef Full Text | Google Scholar
Titov, N., Dear, B. F., McMillan, D., Anderson, T., Zou, J., and Sunderland, M. (2011). Psychometric comparison of the PHQ-9 and BDI-II for measuring response during treatment of depression. Cogn. Behav. Ther. 40 (2), 126–136. doi:10.1080/16506073.2010.550059
PubMed Abstract | CrossRef Full Text | Google Scholar
Turner, S. M., Beidel, D. C., Long, P. J., and Greenhouse, J. (1992). Reduction of fear in social phobics: an examination of extinction patterns. Behav. Ther. 23, 389–403. doi:10.1016/s0005-7894(05)80165-0
CrossRef Full Text | Google Scholar
Üstün, T. B., Chatterji, S., Kostanjsek, N., Rehm, J., Kennedy, C., Epping-Jordan, J., et al. (2010). Developing the world health organization disability assessment schedule 2.0. Bull. World Health Organ. 88, 815–823. doi:10.2471/blt.09.067231
PubMed Abstract | CrossRef Full Text | Google Scholar
Weathers, F. W., Litz, B. T., Keane, T. M., Palmieri, P. A., Marx, B. P., and Schnurr, P. P. (2013) “The PTSD checklist for DSM-5 (PCL-5),” in Scale available from the national center for PTSD at. Available at: https://www.ptsd.va.gov.
Google Scholar
Zwertig, S. E., Koch, L. M., Blount, T. H., Graham, M. M., and Peterson, A. L. (2022). Massed prolonged exposure for PTSD in two firefighters: preliminary case study findings. Behav. Modif. 46 (3), 427–452. doi:10.1177/01454455211011977
PubMed Abstract | CrossRef Full Text | Google Scholar